Understanding Legionnaires’ Disease: Symptoms, Prevention, and Treatment
Legionnaires’ disease is a severe form of pneumonia that can pose serious health risks, particularly for vulnerable populations. Caused by Legionella bacteria, this illness is often misunderstood, yet it’s entirely preventable and treatable with the right knowledge and actions. In this comprehensive guide, we’ll explore what Legionnaires’ disease is, its symptoms, risk factors, causes, prevention strategies, testing, treatment, and potential complications. Whether you’re a homeowner, a building manager, or simply curious about this condition, this article provides actionable insights to keep you informed and safe.
Understanding these basics sets the stage for diving deeper into what makes this disease unique and how to manage its risks effectively.
What Is Legionnaires’ Disease?
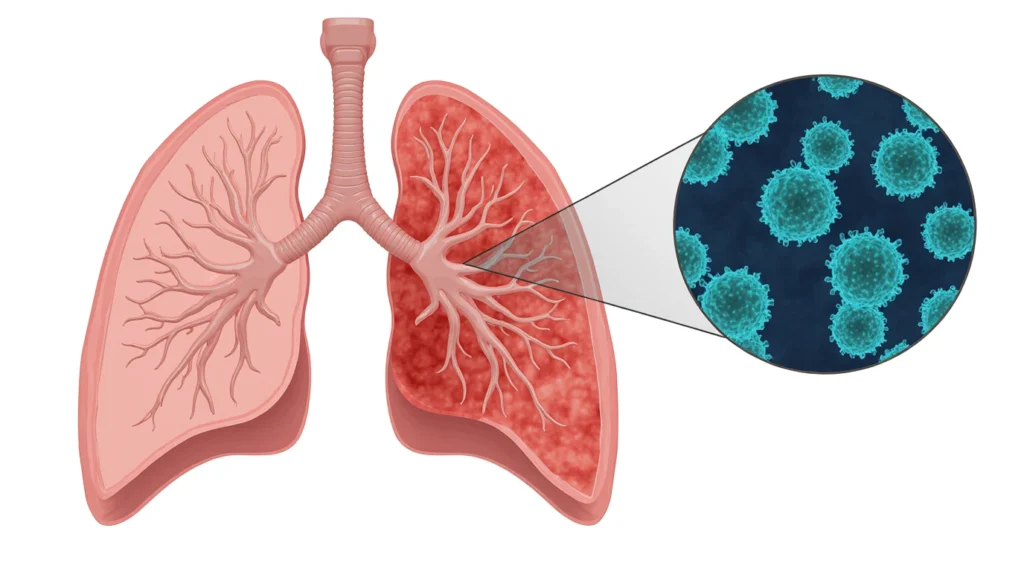
Legionnaires’ disease is a severe form of pneumonia—a lung infection that inflames the air sacs, making breathing difficult. It’s caused by Legionella bacteria, which thrive in warm, stagnant water environments like cooling towers, hot water tanks, and plumbing systems. The disease was first identified in 1976 during an outbreak at an American Legion convention in Philadelphia, which is how it got its name.
Legionella bacteria can cause two distinct illnesses:
- Legionnaires’ disease: A severe pneumonia that can lead to hospitalization and, in some cases, life-threatening complications.
- Pontiac fever: A milder, flu-like illness that typically resolves on its own without treatment.
While Pontiac fever is less concerning, Legionnaires’ disease requires prompt medical attention due to its potential severity. Both conditions arise from exposure to Legionella, but their impact on the body differs significantly.
Table of Contents
Symptoms of Legionnaires’ Disease
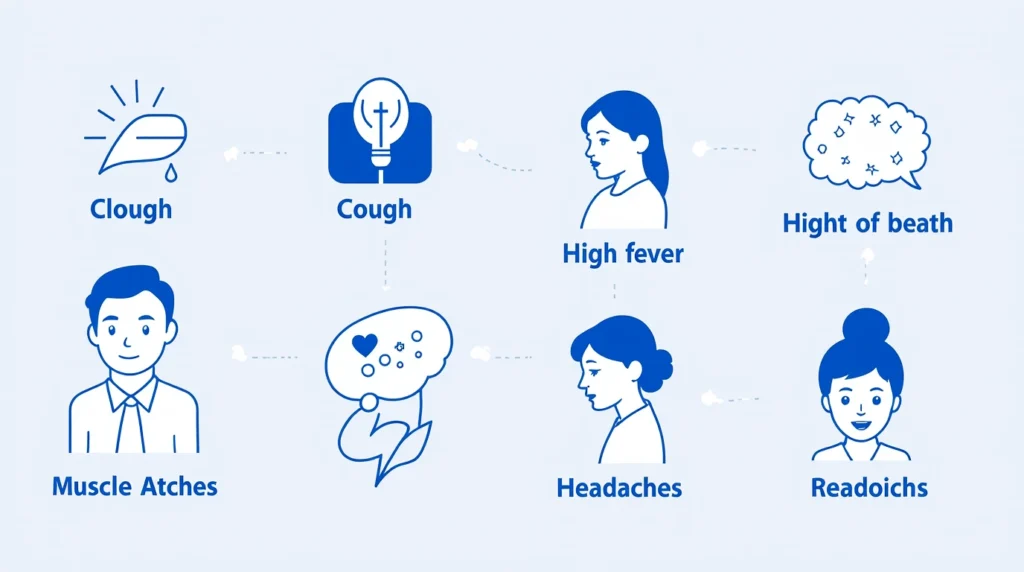
The symptoms of Legionnaires’ disease typically appear 2 to 14 days after exposure to Legionella bacteria. Because they mimic other types of pneumonia, it’s easy to overlook them without proper testing. Recognizing these signs early can make a significant difference in treatment outcomes.
Common Symptoms
- Cough: Often dry at first, but may produce mucus or blood as the infection progresses.
- High fever: Temperatures can reach 104°F (40°C) or higher, accompanied by chills.
- Headaches: Persistent and sometimes severe.
- Muscle aches: Generalized body pain that feels similar to the flu.
- Shortness of breath: Difficulty breathing, especially during physical activity.
Additional Symptoms
Some individuals may experience:
- Confusion: Particularly in older adults, which can be mistaken for other conditions like dementia.
- Diarrhea: Loose stools or digestive upset.
- Nausea: Feeling queasy or vomiting.
If you or someone you know develops these symptoms, especially after potential exposure to contaminated water sources (like a recent stay in a hotel or hospital), seek medical care promptly. Early intervention is key to preventing complications.
Risk Factors for Legionnaires’ Disease
While Legionella bacteria are widespread in natural water sources, most healthy people exposed to them don’t develop Legionnaires’ disease. However, certain factors increase the likelihood of illness, particularly for those with compromised health.
Who’s at Risk?
- Older adults: People aged 50 and older are more susceptible due to age-related declines in immune function.
- Smokers: Current or former smokers have damaged lungs, making them more vulnerable to infection.
- People with chronic lung conditions: Those with COPD, emphysema, or asthma face higher risks.
- Individuals with weakened immune systems: This includes people with HIV/AIDS, cancer, or those taking immunosuppressive medications (e.g., after organ transplants).
- Those with underlying conditions: Diabetes, kidney disease, or liver disease can increase susceptibility.
Environmental Risk Factors
Exposure is more likely in settings where Legionella can proliferate, such as:
- Large buildings with complex water systems (e.g., hotels, hospitals, or office buildings).
- Hot tubs, fountains, or cooling towers that aren’t properly maintained.
- Cruise ships or resorts with shared water systems.
Understanding these risk factors can help you take proactive steps to minimize exposure, especially if you or a loved one falls into a high-risk group.
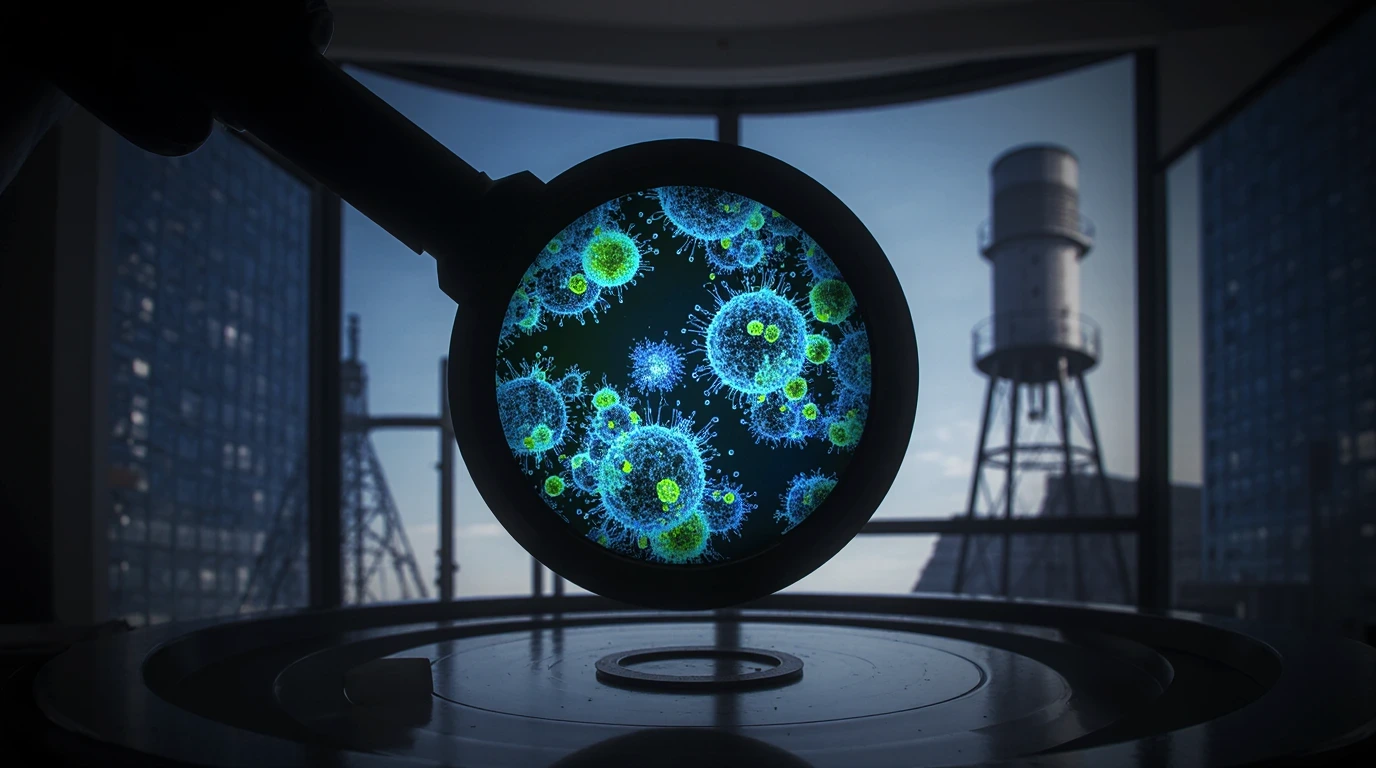
Causes of Legionnaires’ Disease

Legionnaires’ disease is caused by Legionella bacteria, which are naturally found in freshwater environments like lakes and streams. However, they become a health hazard when they multiply in human-made water systems where conditions are ideal for growth—warm temperatures (77°F to 113°F or 25°C to 45°C), stagnant water, and the presence of nutrients like biofilm.
How It Spreads
People contract Legionnaires’ disease by inhaling tiny droplets of water (mist or vapor) containing Legionella. Common sources include:
- Cooling towers: Used in air conditioning systems for large buildings.
- Hot tubs and spas: If not properly disinfected.
- Showerheads and faucets: Especially in older buildings with outdated plumbing.
- Decorative fountains: Often found in public spaces.
- Humidifiers or nebulizers: If filled with contaminated water.
Importantly, Legionnaires’ disease is not spread from person to person, nor is it typically contracted by drinking contaminated water. The primary risk comes from breathing in aerosolized droplets.
Prevention of Legionnaires’ Disease
Preventing Legionnaires’ disease hinges on controlling the growth and spread of Legionella bacteria in water systems. Whether you’re a building manager, homeowner, or individual, there are practical steps you can take to reduce the risk.
For Building Owners and Managers
Large buildings with complex water systems are prime breeding grounds for Legionella. To prevent outbreaks:
- Develop a water management plan: Follow guidelines from the CDC or local health authorities to identify and mitigate risks.
- Maintain proper water temperatures: Keep hot water above 140°F (60°C) and cold water below 68°F (20°C).
- Regularly clean and disinfect cooling towers, hot tubs, and plumbing systems.
- Flush unused water systems: Run taps and showers in vacant buildings to prevent stagnation.
- Test water systems: Periodically check for Legionella contamination, especially in high-risk facilities like hospitals.
For Homeowners
While the risk is lower at home, you can still take precautions:
- Clean and maintain hot tubs: Follow manufacturer guidelines for disinfection and water changes.
- Flush stagnant water: Run faucets and showers after long periods of disuse (e.g., after a vacation).
- Service water heaters: Keep them at 140°F (60°C) to inhibit bacterial growth.
- Use sterile water in medical devices: For humidifiers or CPAP machines, use distilled or sterile water.
For Individuals
- Avoid high-risk areas: Be cautious around poorly maintained hot tubs or decorative fountains.
- Use proper windshield washer fluid: In motor vehicles, use commercial washer fluid rather than tap water, as Legionella can grow in stagnant reservoirs.
- Stay informed: If you’re in a high-risk group, be vigilant about symptoms after potential exposure.
By implementing these measures, you can significantly reduce the chances of Legionella exposure in both public and private settings.
Testing and Diagnosis

Diagnosing Legionnaires’ disease can be challenging because its symptoms resemble other types of pneumonia. A combination of clinical evaluation and specialized tests is required to confirm the diagnosis.
Diagnostic Process
- Chest X-ray: Used to detect pneumonia by showing inflammation or fluid in the lungs.
- Laboratory Tests:
- Urine antigen test: The most common test, which detects Legionella proteins in urine. It’s quick and reliable but only identifies certain strains.
- Sputum or lung fluid culture: A sample is tested in a lab to grow Legionella bacteria, confirming the diagnosis.
- Blood tests: These may show elevated white blood cell counts, indicating infection.
- Medical history review: Doctors ask about recent travel, exposure to water systems, or stays in healthcare facilities.
Reporting
Confirmed cases of Legionnaires’ disease are reported to local or state health departments. This helps track outbreaks and identify contaminated water sources, protecting public health.
If you suspect Legionnaires’ disease, seek medical attention immediately. Prompt testing ensures faster treatment and better outcomes.
Treatment and Recovery
Legionnaires’ disease is treatable, but it requires specific antibiotics to target Legionella bacteria. Unlike viral pneumonia, it doesn’t respond to over-the-counter medications or rest alone.
Treatment Approach
- Antibiotics: Common options include azithromycin or levofloxacin, administered orally or intravenously depending on severity.
- Hospitalization: Many patients, especially those with severe symptoms or underlying conditions, require hospital care for IV antibiotics and oxygen support.
- Supportive care: Fluids, fever reducers, and respiratory therapy help manage symptoms.
Recovery Outlook
- Most patients recover fully with timely treatment, though recovery can take weeks.
- Early treatment is critical: Delays can lead to complications, particularly in high-risk individuals.
- Hospital stays vary: Some patients are discharged within days, while others with severe cases may need longer care.
Even healthy individuals often require hospitalization due to the disease’s intensity. Follow-up care, including rest and hydration, is essential for a full recovery.
Complications of Legionnaires’ Disease
While most people recover with treatment, Legionnaires’ disease can lead to serious complications, especially in severe cases or when treatment is delayed.
Potential Complications
- Respiratory failure: The lungs may struggle to provide enough oxygen, requiring mechanical ventilation.
- Septic shock: A life-threatening drop in blood pressure caused by widespread infection.
- Kidney failure: The infection can impair kidney function, sometimes requiring dialysis.
- Death: The mortality rate is approximately 1 in 10 for all cases and 1 in 4 for healthcare-associated infections.
Vulnerable Populations
Complications are more likely in:
- Older adults.
- Those with pre-existing lung or immune system conditions.
- Patients who contract the disease in healthcare settings, where bacteria may be more resistant.
These risks underscore the importance of prevention and early intervention to minimize the disease’s impact.
Conclusion: Staying Safe from Legionnaires’ Disease

Legionnaires’ disease, caused by Legionella bacteria, is a serious but manageable health concern. By understanding its symptoms, risk factors, and causes, you can take proactive steps to protect yourself and others. Prevention is key—whether it’s maintaining water systems, avoiding high-risk environments, or using proper precautions in vehicles. If symptoms arise, prompt testing and diagnosis followed by treatment with antibiotics can lead to a full recovery for most people. However, awareness of potential complications highlights the need for vigilance, especially for those at higher risk.
Stay informed, stay cautious, and prioritize water safety to keep Legionnaires’ disease at bay. If you manage a building or belong to a high-risk group, take action today to reduce your exposure and ensure peace of mind.