Sweating as a Side Effect of SSRIs: Unpacking the Biological Mechanism, Persistent Challenges, and Treatment Options
Introduction
Imagine this: It’s a mild spring day, the kind where everyone else is comfortably strolling around in light jackets, but you’re drenched in sweat as if you’ve just finished a marathon. Your shirt clings to your back, beads of perspiration trickle down your forehead, and you can’t help but feel self-conscious in social situations. This isn’t just a random hot flash or the result of overexerting yourself—it’s a daily reality that’s become all too familiar. For me, it started subtly a few months after I began taking an SSRI (Selective Serotonin Reuptake Inhibitor) for anxiety. At first, I brushed it off as stress or maybe the weather, but soon it escalated to the point where even sitting in an air-conditioned room left me feeling like I was in a sauna.
What I didn’t realize initially was that this excessive sweating was directly linked to my medication. SSRIs, commonly prescribed for depression, anxiety, and other mental health conditions, can trigger a range of side effects, and sweating is one of the more disruptive ones. It’s not uncommon; in fact, many people on these meds experience it to varying degrees. If you’re reading this, you might be in the same boat—searching for answers on why this happens and what you can do about it. In this article, we’ll dive deep into sweating as a side effect of SSRIs, exploring the biological mechanism involving the hypothalamus and serotonin, why it’s often a persistent side effect, available treatment options like adjusting dosage or switching meds, and some self-care strategies along with encouragement to keep going.
Sweating as a side effect isn’t just an annoyance; it can impact your quality of life, from work meetings to intimate moments. But understanding the “why” behind it can empower you to seek solutions. Let’s break it down step by step, starting with the science of how SSRIs influence your body’s sweat response.

Why SSRIs Make You Sweat More
SSRIs work by increasing the levels of serotonin in your brain, which helps regulate mood and alleviate symptoms of depression and anxiety. However, this boost in serotonin doesn’t stay confined to mood regulation—it can spill over into other bodily functions, including how your body manages temperature and sweating. Studies show that sweating as a side effect affects anywhere from 5% to 14% of people taking SSRIs. That’s a significant portion, meaning if you’re experiencing this, you’re far from alone. This statistic comes from clinical reviews and patient reports, highlighting how common yet under-discussed this issue is in mental health treatment.
To understand the root cause, we need to look at the biological mechanism behind it. Dr. Ludmila De Faria, a psychiatrist and expert in psychopharmacology, explains that SSRIs impact the brain’s hypothalamus, a small but mighty region that acts as the body’s internal thermostat. The hypothalamus is responsible for maintaining your core body temperature, signaling when to sweat to cool down or shiver to warm up. It’s like the control center in a smart home, constantly adjusting to keep everything balanced.
When you take an SSRI, it inhibits the reuptake of serotonin, leading to higher levels of this neurotransmitter in the synapses. While that’s great for mood, excess serotonin in the hypothalamus can disrupt its normal functioning. Serotonin plays a role in thermoregulation, and too much of it can make the hypothalamus overly sensitive. As a result, your body might perceive even minor temperature changes or stressors as threats that require aggressive cooling. This leads to profuse sweating, even in situations where it wouldn’t normally occur—like during a casual conversation or while watching TV.
Think of it this way: Normally, your body’s cooling system is calibrated precisely, like a well-tuned air conditioner that kicks in only when needed. But with elevated serotonin levels, it’s as if someone cranked up the sensitivity dial, causing the system to overreact and flood the room (or in this case, your skin) with unnecessary coolant. This biological mechanism involving the hypothalamus and serotonin is why sweating becomes more frequent and intense for some SSRI users.
Unfortunately, this isn’t a side effect that typically fades over time. Many people hope that their body will adjust after a few weeks or months, but sweating as a side effect is often a persistent side effect. Research indicates that while some initial side effects like nausea or headaches may diminish as your body acclimates, thermoregulatory issues like excessive sweating tend to stick around. This persistence can be frustrating, especially if the medication is otherwise effective for your mental health. It’s not that your body can’t adapt at all—some individuals report slight improvements—but for most, it remains a steady companion unless addressed directly.
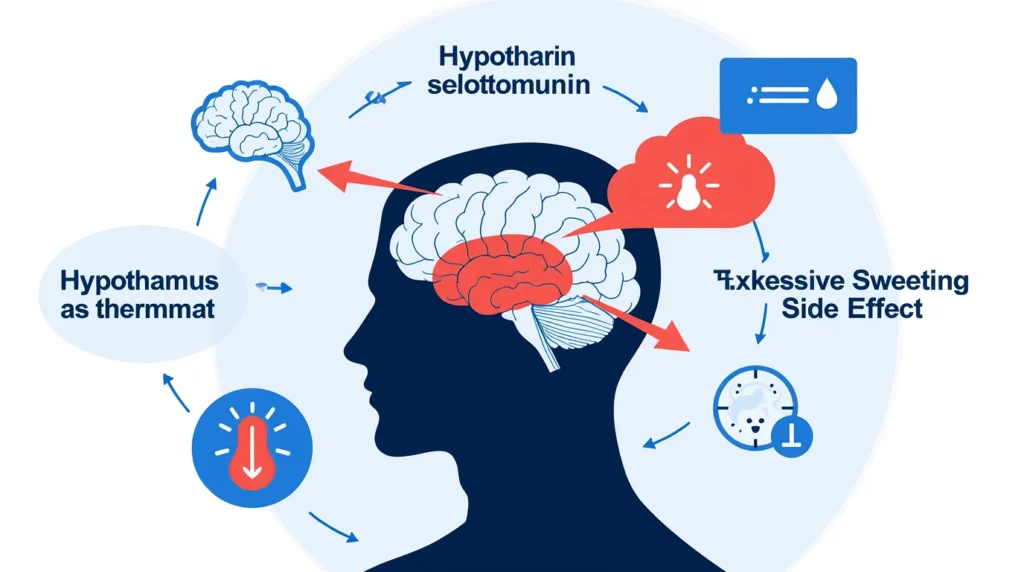
Delving deeper into the science, the hypothalamus isn’t working in isolation. It’s part of the broader autonomic nervous system, which controls involuntary functions like heart rate and digestion. Serotonin’s influence here can create a cascade effect: heightened serotonin receptors in the hypothalamus signal the sweat glands via the sympathetic nervous system, leading to hyperhidrosis (excessive sweating). This can manifest as generalized sweating or focal areas like the palms, underarms, or face.
Personal stories abound in online forums and support groups. One user shared how their SSRI-induced sweating turned a simple grocery run into an embarrassing ordeal, with sweat dripping visibly despite cool weather. Another described night sweats that disrupted sleep, adding to the fatigue already associated with depression. These anecdotes underscore the real-world impact of this biological mechanism.
Moreover, factors like dosage, individual genetics, and even concurrent medications can exacerbate the issue. Higher doses often correlate with more pronounced sweating, as more serotonin floods the system. Genetic variations in serotonin transporters might make some people more susceptible. And if you’re on other drugs that affect serotonin, like certain painkillers or supplements, the risk amplifies.
In essence, the interplay between SSRIs, the hypothalamus, and serotonin creates a perfect storm for sweating as a side effect. Recognizing this persistent side effect is the first step toward managing it effectively. Now, let’s explore practical steps you can take to mitigate it.
What You Can Do About It

Facing sweating as a side effect doesn’t mean you’re stuck with it forever. There are several treatment options available, though they should always be pursued under medical supervision. The goal is to balance effective mental health management with minimizing discomfort. Let’s discuss the key strategies, starting with dosage adjustments.
One of the simplest treatment options is to lower the dosage of your current SSRI. This can reduce the intensity of side effects like sweating without completely sacrificing the therapeutic benefits. For instance, if you’re on a higher dose to combat severe symptoms, your doctor might suggest tapering down gradually to find a sweet spot where mood stabilization remains intact, but the serotonin overload on the hypothalamus is lessened. However, this must be done with a doctor’s approval—abrupt changes can lead to withdrawal symptoms or a resurgence of depression/anxiety.
Clinical guidelines from organizations like the American Psychiatric Association emphasize monitoring side effects closely. In one study, patients who reduced their SSRI dosage reported a 20-30% decrease in sweating incidents, though results vary. It’s worth discussing this with your prescriber, perhaps tracking your sweating episodes in a journal to provide concrete data. Factors like your overall health, duration on the medication, and response history will influence whether this is viable.
If lowering the dosage isn’t enough or compromises efficacy, switching to a different medication emerges as another strong treatment option. Not all SSRIs affect everyone the same way due to subtle differences in their chemical structures and how they interact with serotonin receptors. For example, while fluoxetine (Prozac) might trigger heavy sweating in one person, sertraline (Zoloft) or escitalopram (Lexapro) could be better tolerated. Switching meds allows you to trial alternatives within the SSRI class or even to other antidepressants like SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors) if needed.
Dr. De Faria and other experts note that this trial-and-error process is common in psychiatry. It might take a few attempts, but many patients find relief. A meta-analysis of antidepressant side effects showed that switching reduced thermoregulatory issues in about 40% of cases. Your doctor can guide the transition, often with a cross-taper method to minimize disruptions. Be patient—full effects can take weeks.
That said, avoid self-medicating or using over-the-counter remedies without advice. Specifically, steer clear of anticholinergic drugs, which are sometimes used for hyperhidrosis but can interfere with SSRIs. These medications block acetylcholine, a neurotransmitter involved in sweating, but they come with risks like “brain fog”—that hazy, forgetful feeling that can worsen cognitive side effects already possible with SSRIs. Other downsides include dry mouth, constipation, and urinary issues, making them less ideal for long-term use in this context.
Beyond pharmacological tweaks, consider lifestyle integrations as part of your treatment options. While not a cure, combining medical adjustments with habits can amplify relief. For persistent side effects, some turn to specialized treatments like botox injections for focal sweating or iontophoresis (a device that uses electrical currents to reduce sweat gland activity), but these are typically for severe cases and require dermatologist input.
Therapy can also play a role. Cognitive Behavioral Therapy (CBT) might help manage the emotional toll of sweating, reducing stress that could exacerbate it. And don’t overlook consulting a specialist—if your primary care doctor isn’t addressing this adequately, a psychiatrist or endocrinologist might offer deeper insights into the biological mechanism at play.
In summary, treatment options like adjusting dosage or switching meds provide hope for alleviating this persistent side effect. With professional guidance, you can navigate these changes safely and effectively.

Conclusion
While dealing with sweating as a side effect of SSRIs can feel overwhelming, incorporating self-care strategies can make a noticeable difference in your daily comfort. Start with the basics: Stay hydrated by drinking plenty of water throughout the day. Dehydration can worsen sweating, as your body works harder to regulate temperature. Aim for at least 8-10 glasses, more if you’re active or in warm environments. Opt for breathable clothing made from natural fabrics like cotton or moisture-wicking materials to help evaporate sweat faster and reduce that clammy feeling.
Avoid intense heat exposure whenever possible. This means scheduling outdoor activities for cooler parts of the day, using fans or air conditioning indoors, and steering clear of spicy foods or caffeine, which can trigger sweat responses. Simple tweaks like these support your body’s natural efforts to cope with the disrupted thermoregulation caused by excess serotonin in the hypothalamus.
On a broader note, remember that managing mental health is a journey, and finding the right medication is part of that natural process. It’s okay if it takes time—many people go through adjustments before landing on what works best. You’re taking proactive steps by educating yourself about the biological mechanism, recognizing the persistent side effect, and exploring treatment options like dosage changes or switching meds. This persistence is a sign of strength, and with self-care and encouragement from supportive communities, you’ll navigate this hurdle.
If sweating persists despite efforts, don’t hesitate to loop back with your healthcare provider. Resources like patient advocacy groups or online forums can offer additional encouragement, reminding you that relief is achievable. Hang in there; the path to balance is worthwhile, and brighter, drier days are ahead.







